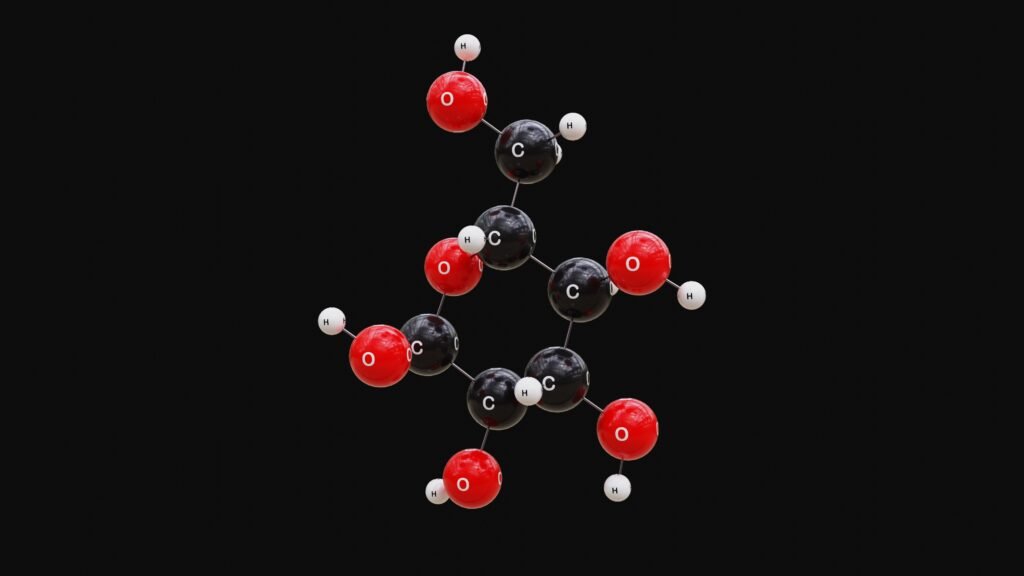
Managing diabetes effectively requires more than just medication and diet—it also demands regular blood glucose monitoring. Knowing your blood sugar levels helps you make informed decisions about food, exercise, and medication, and it can prevent serious complications.
Whether you have Type 1, Type 2, or gestational diabetes, consistent monitoring is key to long-term health.
In this blog, we’ll explore why blood glucose monitoring is essential, the best tools available in 2024, and practical techniques to make the process easier.
Why Blood Glucose Monitoring Matters
Your blood sugar levels fluctuate throughout the day, influenced by meals, physical activity, stress, and medication. Without regular monitoring, you may not notice dangerously high or low levels until symptoms become severe.
Benefits of Regular Monitoring:
- Helps prevent hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar)
- Tracks how your body responds to different foods and activities
- Supports better medication adjustments
- Provides critical data for your healthcare provider
- Empowers you to manage your condition proactively
Recommended Blood Sugar Targets
Blood sugar targets can vary based on your health status and doctor’s recommendations, but typical goals are:
- Before Meals: 80 to 130 mg/dL
- Two Hours After Meals: Less than 180 mg/dL
- A1C (3-Month Average): Below 7% (may vary per individual)
Monitoring helps you stay within these target ranges and detect patterns that need adjustment.
Blood Glucose Monitoring Tools
1. Traditional Blood Glucose Meters (BGM)
These devices use a small drop of blood (usually from your fingertip) to measure your glucose levels.
Pros:
- Affordable
- Easy to use
- Widely available
Cons:
- Requires multiple finger pricks daily
- Can feel inconvenient or painful over time
2. Continuous Glucose Monitors (CGM)
CGMs use a small sensor placed under the skin to provide real-time glucose readings throughout the day and night.
Pros:
- Provides continuous tracking
- Sends alerts for high or low readings
- Reduces the need for finger pricks
Cons:
- More expensive
- Requires sensor changes every 7-14 days
- May need calibration with fingerstick tests
Popular CGM devices in 2024 include Dexcom G7, FreeStyle Libre 3, and Medtronic Guardian Connect.
3. Smartphone-Integrated Monitors
Many glucose meters and CGMs now sync with smartphone apps, allowing you to:
- Track readings over time
- Share data with your healthcare provider
- Set reminders and alerts
These integrations make it easier to spot trends and manage your diabetes on the go.
How Often Should You Check?
The frequency of blood sugar checks depends on:
- Type of diabetes: Type 1 often requires more frequent checks than Type 2.
- Treatment plan: If you use insulin, you may need to test before meals and bedtime.
- Activity level: More frequent testing is recommended when exercising or adjusting medication.
- Doctor’s advice: Your healthcare provider will give personalized guidance.
Tips for Successful Monitoring
- Be Consistent: Test at the same times daily to track reliable trends.
- Record Your Results: Use a logbook or mobile app to note readings, meals, activity, and medication.
- Rotate Testing Sites: To avoid sore fingertips, rotate fingers or use other approved sites.
- Understand the Numbers: Learn what causes highs and lows so you can take corrective action.
- Carry Your Supplies: Always have your meter, strips, and a fast-acting sugar source with you.
When to Seek Help
Contact your doctor if you experience:
- Frequent high or low readings
- Unexplained dizziness, fainting, or severe fatigue
- Symptoms of diabetic ketoacidosis (nausea, fruity breath, confusion) in Type 1 diabetes
Timely adjustments to your treatment plan can prevent long-term complications.
Blood glucose monitoring is a cornerstone of effective diabetes management. It provides immediate feedback, empowers you to make smart daily choices, and helps your healthcare team fine-tune your care.
Whether you’re using a traditional meter or a modern CGM, staying on top of your numbers can significantly improve your quality of life and prevent diabetes-related emergencies.
Embrace the technology, stay informed, and make monitoring a regular part of your routine—it’s one of the most powerful tools you have in your diabetes journey.